Waves of Change in the Type 2 Diabetes Research – and Microbial Gut — Community
April 17, 2023
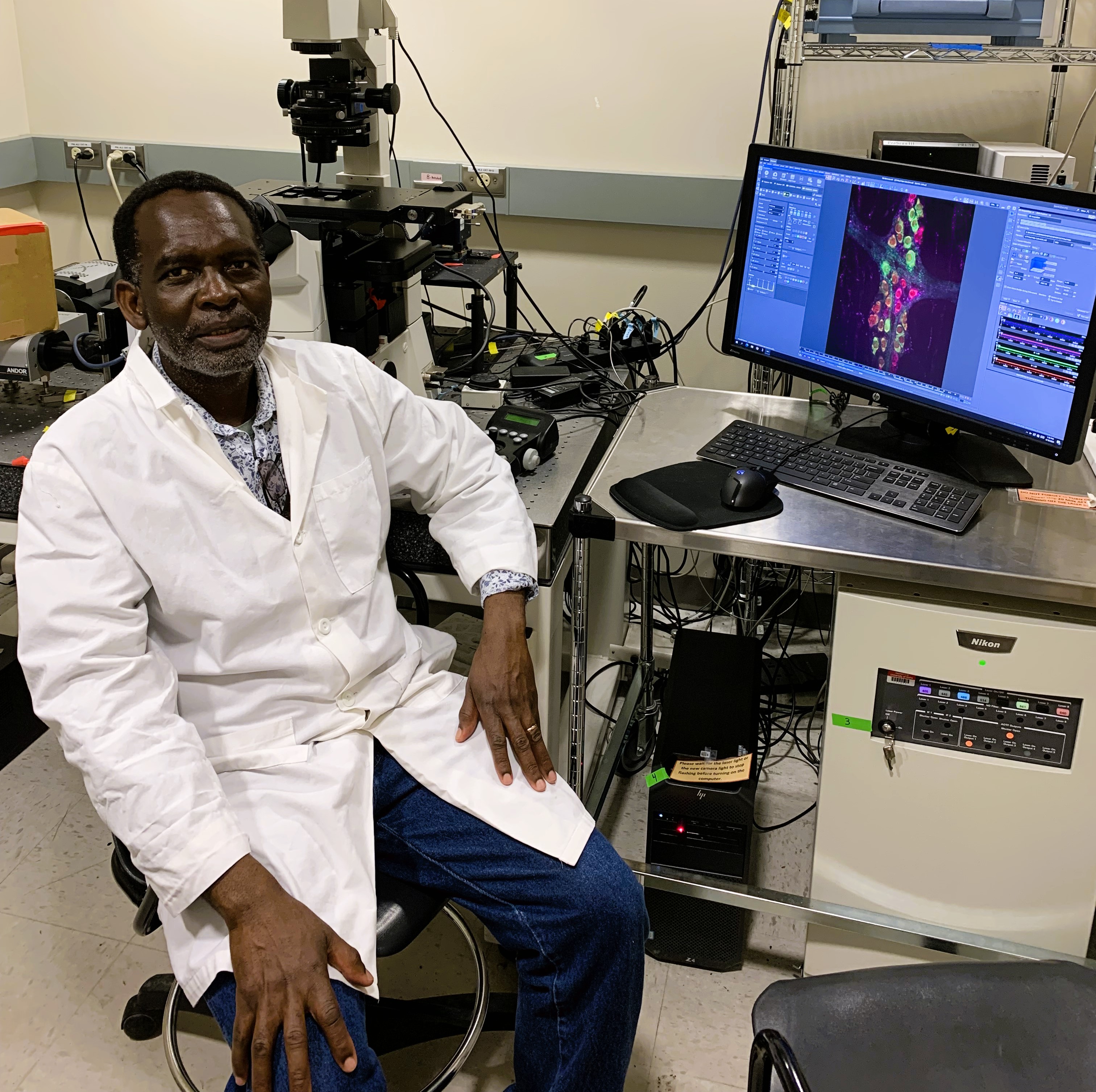
Onesmo Balemba’s fascination with the pathogenesis of gastrointestinal diseases began at an early age in Tanzania.
"There is a trigger for everything," says Balemba, reflecting on the origins of his winding journey to becoming an expert in gastrointestinal system. "While growing up as a kid, I used to hear my mother complaining about bowel pain. I wanted to do something to understand its causes and help my mother. I wanted to become a medical doctor."
He never did become a medical doctor, but he did become a veterinarian and an expert in gastrointestinal (GI) physiology and pathophysiology of GI diseases. He now works on identifying the link between the gut microbiota and type 2 diabetes at the University of Idaho as a full professor with his own lab.
In February 2023, Balemba and other scientists and bioinformatics experts at the U of I identified a list of species of bacteria involved in Type 2 Diabetes. The study provides the most detailed accounts of the differences in reversed prediabetes, pre-diabetes and type 2 diabetes microbiomes to date.
An Unexpected Journey
Balemba earned a bachelor's degree in veterinary medicine and joined the Tanzanian government initiative to crossbreed cattle, where he regularly woke up at 4 a.m. to start his rounds at a ranch with thousands of cattle and hundreds of water buffalo, goats, sheep and horses.
Two years of this was enough hard labor to prompt him to return to academia. He switched to teaching in the Faculty of Veterinary Medicine at the Sokoine University of Agriculture (SUA) in Tanzania and stayed there for ten years. He then earned a master’s and Ph.D. in veterinary medicine via a joint program between SUA and the Royal Veterinary and Agriculture University in Copenhagen, where he could perform experiments in Tanzania on the mechanisms of pain in diarrhea and schistosome-induced injury to the enteric nervous system or the "gut-brain," and analyze his results in Copenhagen.
After postdoctoral training in the United States, he arrived in Moscow in 2008 with a strong understanding of the GI system. Fourteen years later, he has learned enough through his research that he is able to make complex connections between the gut microbiota, damage to the "gut-brain," and altered GI movements in type 2 diabetes.
Still, says Balemba, “It [diabetes] is a very complex disease. If we knew all the causes, we would have found a cure.â€
Classifying Type 2 Diabetic Microbiota
"Most people know that GI dysfunction in type 2 diabetes can come from prolonged high blood sugar levels. But our hypothesis is that this dysfunction comes from diet-induced shifts in the gut microbiota that happen before people have symptoms of diabetes."
The idea is that shifts in microbiota in people with type 2 diabetes damage the gut-brain by eliciting the production of endotoxins that live in bacterial cell walls. When digestion slows, the toxic substances from the gut including bacterial products are released more readily into the bloodstream, causing inflammation and impairing how the body uses glucose.
In 2022, Balemba began working with U of I Bioinformatics Data Scientist Sarah Hendricks to characterize the microbiome of diabetic patients – the first step to testing his hypothesis. Hendricks was able to sequence long portions of bacteria extracted from diabetic, pre-diabetic, reverse diabetic and healthy patients. She uses a powerful, expensive machine called the PacBio Sequel II Genome Sequencer.
"With a longer portion, you can start to tell the differences between bacterial species and between strains. That was a big part of what had never been done before," says Hendricks. Their paper was published in February.
It was an exciting moment for Balemba to discover specific members of microbial communities of diabetic patients. Linking these species to their effects on the nervous system would be a huge step forward for researchers and the medical community.
Linking the Gut-Brain Axis
The next step in Balemba’s research focuses on the toxins that trigger the GI system to slow down. To see if these toxins accumulate before the patient develops type 2 diabetes, Balemba extracted and filtered stool from 47 participants and transplanted them into healthy mice. After the filtrates had been running through the mice for eight weeks, he analyzes their effects on the “gut brain,†GI movements, inflammation and insulin resistance.
Although the results are not published yet, he saw surprisingly dramatic results when he treated the isolated intestinal muscle preparations with the filtrates. In fact, the contractions nearly completely halted after just 24 hours.
When asked if he feels like he understands his mother’s bowel pain he witnessed as a kid, he pauses and sits back in his chair. “I have done what I can do. I don’t think I have reached my potential,†he says.
He says this despite decades of research on gastrointestinal disease and extensive study on novel compounds in Garcinia buchanani stem back extract, which is used to mitigate diarrhea and bowel pain.
“But now I am excited about this project,†says Balemba. “We are investigating a very important process that can potentially change the way we view and treat type 2 diabetes.â€
With the help of bioinformatics experts like Hendricks, Balemba is certainly making strides to doing so.
By Kelsey Swenson, IIDS Scientific Writing Intern